3.5 FAMILY WELFARE
3.5.52 The Family
Welfare Programme has made considerable progress during the last few
decades, more so during the last decade. 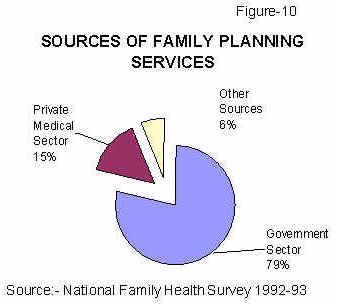
3.5.53 The major lessons learnt during this period are:
-
In spite of obvious constrains and inadequacies, the governmental network can, and does, provides most of the MCH and contraceptive care (Figure 10);
-
Adequate financial inputs and health infrastructure are essential prerequisites for the success of the programme; substantial improvement in achievement of MCH and FP targets occurred when funds were provided (Table 3.5.7 and Table 3.5.2);
- Providing integrated MCH and contraceptive care ensures not only efficient and effective delivery of services but also helps in building up rapport with the families and the community so essential to sustain the FW programme;
- Counselling and education are powerful tools to overcome the barriers of poverty, ignorance, illiteracy and conservative social mores for achieving the small family norm;
- The population is conservative but is responsible, responsive and mature; its response to rapidly changing birth and death rates and availability of services might be initially slow but it is rational and once developed, is sustainable.
3.5.54 The task ahead of the country during the next decade is to bring about a convergence of all these favourable factors so that the twin goals of small healthy family and sustainable population growth are achieved within a decade.
Population Projection for 1996 –2016 – implications to the FW Programme
3.5.55 Population projections for the period 1996-2016 have been worked out by the Technical Committee on Population Projections under the Chairmanship of Registrar General of India. The age and sex wise distribution of the population for the period 1971-1991 based on census data and the projected population for the period from 2001 upto 2016 is shown in Figure 11. There will be massive increase of population in the 15-59 age group (from 500 million to 800 million) in just twenty years (Figure 12). The RCH care has to provide the needed services for this rapidly growing clientele. Along with the demographic transition, there is concurrent ongoing socioeconomic, educational, information technology transition. The population in this age group will therefore have greater awareness and expectation regarding both the access to a wide spectrum of health care related services and the quality of these services. The Family Welfare Programme has to provide the wider spectrum of health care needs of this population – including maternal and child health care, contraceptive care, management of gynaecological problems, STD/RTI/HIV management and control; quality of services need also be improved. Increasing number of the population beyond 60 years would necessitate provisions for management of some of the major health problems in this age group including management of cancers.
3.5.56 The number of births will not alter substantially over the next two decades; this respite from increasing numbers should be utilised to provide improved access to high quality of services so that there is reduction in the current high IMR and MMR. This in turn might lead to a fall in the current high desired level of fertility. If the birth rate continues to decline at the present rate, replacement level of fertility will not be achieved till 2026. In view of the serious implications of this, efforts should be made to meet all the felt needs for contraception and achieve a more rapid decline in birth rates.
Family Welfare Programme during the Ninth Plan:
3.5.57 During the Ninth Plan period attempts will be made to improve quality and coverage of health care to women, children and adolescents, so that their felt needs for health care are fully met. In addition efforts will be made to improve the participation of men in the planned parenthood movement. Prevention and control of Sexually Transmitted Disease (STD) / Reproductive Tract Infection (RTI) including emerging problem of HIV/AIDS will also receive due attention.
Components of the Reproductive and Child Health Care
Components
of RCH Programme:
|
3.5.58 Comprehensive reproductive and child health care will promote the following:
-
Effective maternal and child health care to ensure safe motherhood and child survival;
- Increased access to contraceptive care to prevent unwanted pregnancies;
- Legal abortion facilities for safe management of unwanted pregnancies;
- Effective nutritional services to vulnerable groups;
- Prevention and treatment of RTI/ STD;
- Reproductive health services for adolescents;
- Prevention and treatment of gynecological problems including infertility, menstrual disorders and prolapse uterus;
- Screening and treatment of cancers, especially that of uterine cervix and breast.
3.5.59 While providing the package of services, efforts will be made to improve the quality of services, make services more responsive to users' needs, ensure that health workers and health care providers have the necessary skills and supplies they need and there is a strong and effective referral system to manage all the risk cases.
Simultaneously the IEC efforts will be directed to:
- Ensure responsible reproductive /sexual behavior;
- Improve awareness about reproductive health needs;
- Promote community participation and optimal utilisation of available services.
3.5.60 Comprehensive RCH services will be made available at all the tertiary and secondary care institutions throughout the country.
Essential Reproductive Health Services
3.5.61 Though it is desirable that the entire package of services indicated above is made available to all those who need it, it will not be possible to immediately implement such a comprehensive package on a nationwide basis. Hence it is envisaged that improvement in quality and coverage of services over and above the existing level will be attempted in all states in an incremental manner so that maternal and child health indices improve.
3.5.62 After consultation with experts a package of essential reproductive health services for nationwide implementation at various levels of health care has been identified. Essential components recommended for nationwide implementation include:
-
Prevention and management of unwanted pregnancy,
-
Services to promote safe motherhood,
-
Services to promote child survival,
-
Prevention and treatment of RTI/STD.
3.5.63 Most of the services are already included in the Family Welfare Programme. However, there are wide variations in the quality and coverage of services not only between states but also between districts in the same state. The focus is therefore on the improvement in the quality and coverage of the services. A project preparation workshop held in Sept. 1995 discussed the issues and problems in implementation of essential RCH package and recommended reproductive and child health services that should be made available at community, sub-centre, PHC and FRU/ District Hospital.
Maternal Care
3.5.64 The major areas of focus of the Safe Motherhood Programme during the Eighth Plan were:
-
Improving maternal care through early registration of pregnant women;
-
Administration of two doses of Tetanus Toxoid (TT) during pregnancy;
-
Providing pregnant women with Iron and Folic Acid (IFA) tablets;
-
Training of Dais for safe delivery especially in districts with high proportion of home deliveries;
-
Provision of Disposable Delivery Kits to those who plan deliveries at home;
-
Improving facilities for antenatal care and safe delivery at sub-centres and PHC; Setting up First Referral Units (FRU) for providing emergency obstetric care and improving referral linkages.
3.5.65 Over the years, there has been a substantial increase in the proportion of pregnant women getting registered (Table 3.5.6). The data reported by Department of Family Welfare indicate that over 70% of pregnant women receive two doses of Tetanus Toxoid (TT) and 100 tablets of Iron and Folic Acid (IFA) during the course of pregnancy. However, maternal morbidity and mortality rates (Figure 6) continue to remain high. To achieve a reduction in these, it is essential to improve the quality of antenatal and intrapartum care. During the Ninth Plan period efforts will be made to ensure that all pregnant women are screened for common problems such as anaemia, infections obstetric problems and the identified `high risk' pregnant women are referred to PHC/ CHC for appropriate management.
3.5.66 Analysis of service data on ANC registration and deliveries reported for the year 1995-96 from 350 districts indicate that there is an increase in the number of hospital deliveries and deliveries attended by trained personnel (Table 3.5.8). In States like Kerala over 90% of deliveries are in institutions and perinatal mortality rates are very low (Table 3.5.9). However, in States like UP, majority of deliveries is at home and are conducted by untrained persons. Consequently, maternal and perinatal mortality rates continue to be high. During the Ninth Plan efforts will be made to promote institutional deliveries both in urban and rural areas. In States where majority of deliveries still occur at home, efforts will be made to train Traditional Birth Attendants (TBAs) through Intensive Dai's Training Programme and to increase availability and access to Disposable Delivery Kits.
3.5.67 Women with problems like Anaemia, malpresentations, suspected Cephalopelvic Disproportion (CPD), Hypertensive Diseases of Pregnancy (HDP) and Gestational Diabetes Mellitus (GDM) should not deliver at home. Screening all women during pregnancy to detect those with such problems and referring them at appropriate time to pre-designated institutions for management and safe delivery will substantially reduce maternal and perinatal morbidity and mortality. The mechanism for screening, as well as referral, will be streamlined during the Ninth Plan period and easy - to - follow protocol will be developed and made available to all health care providers. In "low risk cases", if home delivery is anticipated, provision will be made for aseptic delivery by trained persons. Unpredictable complications can arise even during apparently normal labour; rapid transportation of these women to hospital for emergency obstetric care is essential to reduce morbidity and mortality during delivery. Local Panchayats, NGOs and women's organisations will play an important role in this respect. In the postpartum period early detection and management of infection, support for breast feeding and nutrition counseling will receive due attention.
National Anaemia Prophylaxis programme
3.5.68 India has the dubious distinction of being one of the countries with the highest prevalence of anaemia in the general population. Prevalence of anaemia among pregnant women ranges between 50 -90%. This is mainly due to low intake and poor bio-availability of iron from the diets consumed in India. Poor intake of folic acid and coexisting folate deficiency also contribute to the problem. Anaemia present from childhood through adolescence antedates pregnancy and it gets aggravated during pregnancy and perpetuated by blood loss during labour. Anaemia continues to be responsible for a substantial proportion of the perinatal and maternal morbidity and maternal mortality.
Multi-pronged
Strategy for Prevention and Management of Anaemia in pregnancy
include:
|
3.5.69 Realising the magnitude of the problem, obstetricians made screening and effective management of anaemia an essential component of antenatal care. The National Anaemia Prophylaxis Programme of iron and folic acid distribution to all pregnant women was initiated in 1972 . The implementation and impact of these programmes are being reviewed . Available data from hospital records and information from community-based surveys on prevalence of anaemia in urban and rural population, suggest that the prevalence and the adverse consequences of anaemia in pregnancy have remained essentially unaltered over the past three decades.
3.5.70 Pregnant women with haemoglobin (Hb) less than 8 g/dl show functional decompensation and constitute a high-risk group. The first task is to ensure screening of all pregnant women to identify this high-risk group. A single Hb estimation done around 20th week of pregnancy is sufficient to detect the high-risk anaemic pregnant women. It is essential to evolve a programme for screening all pregnant women for anaemia by Hb estimation utilising the ANM and Lab technicians in the Primary Health Centres so that anaemia in pregnancy could be detected and effectively treated. Unlike the situation elsewhere in the world, oral iron therapy is not effective in correction of the moderate or severe anaemia in Indian pregnant women, because of the poor bio-availability of iron in the Indian diet. Therefore pregnant women with Hb between 5-8 g/dl should be administered appropriate doses of parenteral iron and oral folic acid.
3.5.71 During the Ninth Plan a beginning will be made to use a multi-pronged strategy for prevention and management of anaemia in pregnancy. The programme components aimed at the control of anaemia in pregnancy will include: a) fortification of common foods with iron to increase dietary intake of iron and improve hemoglobin status of the entire population including girls and women prior to pregnancy, b) screening of all pregnant women using a reliable method of hemoglobin estimation for detection of anaemia, c) oral iron folate prophylactic therapy for all non-anaemic pregnant women (Hb > 11 g/dl), d) iron folate oral medication at the maximum tolerable dose throughout pregnancy for women with Hb between 8 and 11 g/dl, e) parenteral iron therapy for women with Hb between 5 and 8 g/dl if they do not have any obstetric or systemic complication, f) hospital admission and intensive personalised care for women with Hb < 5 g/dl, g) screening and effective management of obstetric and systemic problems in all anemic pregnant women and h) improvement in health care delivery system and health education to the community to promote utilisation of available facilities for antenatal and intrapartum care.
Prevention of Unwanted Pregnancy
3.5.72 According to the data available with the Department of Family Welfare as of 31.3.97 45.4% of couples in reproductive age use contraceptives (Table 3.5.1). The data from National Family Health Survey has shown that awareness regarding contraception is nearly universal. But there is an unmet need for contraception (8.5% for terminal methods; 11.0 % for spacing methods) (Table 3.5.4). The Family Welfare Programme will gear itself to meet the `unmet' need during the Ninth Plan period. Vasectomy is safer than tubectomy and efforts will be made to increase acceptance of vasectomy, so that there is substantial reduction in the morbidity associated with terminal methods of contraception. Quality of contraceptive care will be improved. Couples will be provided with balanced information on all available methods of contraception and the advantage and disadvantage of each of these methods so that they choose the method best suited to their needs. Such a balanced presentation and counseling will in the long run not only improve acceptance of contraceptive care, but also improve continuation rates of temporary methods of contraception. The quality of services will be improved through appropriate training of service providers at all levels. During the Ninth Plan efforts will be made to increase involvement of ISM and H practitioners in Family Welfare Programmes. The ISM and H practitioners may provide counseling for couples about contraceptive care and to act as depot holders for OC/ condom. Social marketing will be increasingly utilised to improve access to condoms and oral pills. In addition to the usual channels, the Targeted Public Distribution System (TPDS) outlets may also be used to improve access to condom.
MTP Services
3.5.73 Over two decades have elapsed after the enactment of legislation for Medical Termination of Pregnancy (MTP) act. Over the last two decades the Government of India has taken steps to provide trained manpower and equipment at secondary and primary health care level for safe legal abortion services. The number of MTPs reported to Department of Family Welfare over the last 25 years is shown in Figure13
3.5.74 It is obvious that after the initial rise, the reported number of MTPs has remained below 0.6 million for the last 15 years. In spite of efforts to improve the availability of, and access to, induced abortions services in the primary health care set up, safe abortion services are not available to majority of rural population in India. Even today majority of the estimated 6 million induced abortions are not carried out in settings recognised for legal abortion and about 10% maternal deaths in India are due to septic abortion.
3.5.75 Efforts to improve access to family planning services to reduce the number of unwanted pregnancies and cater to the request for induced abortion will continue to receive intensified attention during the Ninth Plan. In addition, efforts will be made to improve access to safe abortion services by training physicians in MTP and recognising and strengthening institutions which are capable of providing safe abortion services for the first trimester. IEC efforts through appropriate channels of communications to improve awareness among women about availability of safe abortion services at affordable cost through appropriate channels of communication will be intensified. Provision for first trimester abortion will be coupled with appropriate contraceptive care so that these women do not incur the risk of yet another unwanted pregnancy and induced abortion.
RTI AND STD
3.5.76 Sexually Transmitted Diseases (STD) and Reproductive Tract Infections (RTI) continue to be a major public health problem in India. HIV is the most recent addition to the already long list of RTI/STD. So far, there had been no major initiative for detection and management of STD/RTI in women. Sexually transmitted infections in women are usually symptomatic or present with nonspecific symptoms. Even if there are symptoms, women do not go to STD clinics. They seek care in the antenatal, gynecological and family planning clinics. During the Ninth Plan, attempts will be made to provide for screening for syphilis, gonorrhea and HIV infection at PHC/CHC level wherever possible. Utilising the microscope and laboratory technician available at PHCs, vaginal/ cervical smears in women with symptoms of RTI will be screened for identifying organisms responsible and appropriate treatment provided.
Infertility
3.5.77 It is estimated that between 5 to 10% of couples are infertile. While provision of contraceptive advice and care to all couples in reproductive age group is important, it is equally essential that couples who do not have children have access to essential clinical examination, investigation, management and counseling. The focus at the CHC level will be to identify infertile couples and undertake clinical examination to detect the obvious causes of infertility, carry out preliminary investigations such as sperm count, diagnostic curettage and tubal patency testing. Depending upon the findings, the couples may then be referred to centres with appropriate facilities for diagnosis and management. By carrying out simple diagnostic procedures available at the primary health care institutions it is possible to reduce the number of couples requiring referral. Initial screening at primary health care level and subsequent referral is a cost-effective method for management of infertility both for the health care system and those requiring such services.
Gynaecological Disorders
3.5.78 Women suffer from a variety of common gynaecological problems including menstrual dysfunctions at peri-menarchal and peri-menopausal age. Facilities for diagnosis of these are at the moment available at district hospitals or tertiary care centres. During the Ninth Plan period the CHCs, with a gynaecologist, will start providing requisite diagnostic and curative services. Yet another major problem in women is prolapse uterus of varying degrees. The PHCs and CHCs will refer women requiring surgery to district hospitals or tertiary care centres.
3.5.79 Cancer Cervix is one of the most common malignancies in India and accounts for over a third of all malignancies in women. Cancer Cervix can readily be diagnosed at the PHCs and CHCs. Early diagnosis of Stage I and Stage II and referral to places where radiotherapy is available will result in rapid decline in mortality due to Cancer Cervix in the country in the near future.
Maternal Nutrition
3.5.80 The importance of maternal nutrition in determining obstetric outcome has long been recognised. Continued low dietary intake and heavy manual work during pregnancy adversely affect maternal nutrition, course and outcome of pregnancy. The association between low maternal weight, poor pregnancy weight gain and low birth weight has been documented. There is a need to clearly identify pregnant women with moderate and severe undernutrition by weighment and energetic measures should be taken to improve energy balance and weight gain during pregnancy through improved dietary intake, if possible through optimal utilisation of existing food supplementation programmes such as ICDS and through reduction in physical work.
Adolescent Health
3.5.81 The adolescent and youth population in the country is increasing. There are at the moment no specific health or nutrition programmes to address the problem of this important group. In the past teen age pregnancy and its attendant problem were the main focus of attention. Over the years there is a significant rise in age at marriage. Efforts to educate the girl, her parents and the community to delay marriage will continue to receive attention during the Ninth Plan. There is an urgent need to mount programmes for early detection and effective management of nutritional (under-nutrition, anemia) and health (infections, menstrual disorders) problem in adolescent girls. Health and nutrition education to this group is essential.
3.5.82 Adolescent pregnancies are still common in India. Adolescent girls are at high risk of anaemia, HDP and infections. They will receive appropriate care throughout pregnancy and institutional delivery to ensure safety of both the mother and the baby. A scheme "Planned Families by 2000 AD" is being implemented in Andaman and Nicobar islands with the objective of improving literacy, postponing age at marriage and promoting small family norm through financial incentives to the girls in appropriate age groups. If found effective the scheme may be replicated in other areas.
Child Health
3.5.83 Comprehensive, child health services including preventive, promotive and curative services are being provided to those who seek care in secondary and tertiary health care institutions. At primary health care level the spectrum of services available is narrower; focus is mainly on essential new born care, essential child care including ARI and ORT programmes, immunisation, Vit.A and anaemia prophylaxis Programmes. Effective utilisation of available services for prevention and detection of undernutrition in under five population will be the aim of ICDS programme during the Ninth Plan period. Efforts will be focussed on improving quality of screening of children for early detection of health and nutrition problems and improving the referral services so that persons requiring care in secondary and tertiary level institutions receive them without delay.
National Prophylaxis Programme against Nutritional Blindness
3.5.84 In the fifties paediatricians in major hospitals in most of the States reported that Vit A deficiency is a public health problem. Vitamin A deficiency in childhood is mainly due to inadequate dietary intake of Vit A. Increased requirement of the Vit. A due to repeated infection aggravated the magnitude and severity of the deficiency.
| Major
Child Health Care Programmes:
National Prophylaxis Programme against Nutritional Blindness
Child Survival Programme Sustaining and strengthening the ongoing programmes of universal immunisation, ORT, massive dose Vitamin A, Iron Folic Acid supplementation Expanding the coverage of Acute Respiratory Infections (ARI) Control Programme and care of the newborn |
The association between measles, severe PEM and keratomalacia and high fatality in such cases was reported by many paediatricians. Prevalence of night blindness and Bitot's spot in pre-school children ranged between 5% and 10% in most States. Blindness due to Vitamin A deficiency is one of the major causes of blindness in children below 5 years. In view of the serious nature of the problem of blindness due to Vitamin A deficiency it was felt that urgent remedial measures in the form of specific nutrient supplementation covering the entire population of susceptible children should be undertaken. In 1970 the National Prophylaxis Programme Against Nutritional Blindness was initiated as a Centrally Sponsored Scheme (CSS). Under this CSS, all children between ages of one and five years were to be administered 200,000 IU of Vitamin A orally once in six months.
3.5.85 During the last twenty five years this programme had been implemented in all the States and Union Territories. The major bottleneck during the seventies was lack of infrastructure at the peripheral level to ensure timely administration of the massive dose. In the eighties there was considerable improvement in the infrastructure. The lack of adequate doses of Vit A came in the way of improved coverage. Poor orientation of the functionaries who were providing the services to the population, lack of supervision and lack of intersectoral coordination between the health functionaries and the ICDS functionaries persisted throughout the period and has been one of the factors responsible for the continued poor coverage. It is a matter of serious concern that coverage was low in high risk group of children from poorer communities in rural areas and urban slums in poorly performing districts.
3.5.86 In an attempt to improve the coverage especially in the vulnerable 6 months to 23 months age-group, Government of India took a decision to link up Vitamin A administration to the ongoing immunisation programme during the Eighth Plan period. Under the revised regimen a dose of 100,000 IU of Vit.A is to be given to all infants at 9 months along with measles vaccine and a second dose of 200,000 IU is to be administered at 18 months of age along with booster dose of DPT and OPV. Subsequently, the children are to receive three doses of 200,000 IU of Vitamin A every 6 months until 36 months of age. The reported coverage figures under the modified regimen indicate that there has been some improvement in coverage with the first dose (50 -75%). However, the coverage for subsequent doses is low. However, in spite of these short comings , there has been a substantial reduction in the prevalence of blindness due to Vitamin A deficiency from 0.3% in 1971-74 to 0.04% in 1986-89. Repeat surveys carried out by National Nutrition Monitoring Bureau indicated that the incidence of Bitot's spots came down from 1.8% in 1975-79 to 0.7 % in 1988-89.
3.5.87 During the Ninth Plan, every effort will be made to improve the coverage of all doses of massive dose Vit A administration. In addition, health education to improve consumption of foods rich in B-carotene will be continued and backed up by efforts to improve their availability at affordable cost. The target for the Ninth Plan is to control Vitamin A deficiency so that the incidence of blindness due to Vit.A deficiency becomes less than 1/10,000 not only at the national level but also in every State.
Child Survival Programme
3.5.88 During the Eighth Plan period, the Child Survival programme was aimed at reduction of infant and child morbidity and mortality through:
-
Sustaining and strengthening the ongoing programmes of universal immunisation, ORT, massive dose Vitamin A, Iron Folic Acid supplementation and
- Expanding the
coverag
 e
of Acute Respiratory Infections (ARI) Control Programme and care of
the newborn.
e
of Acute Respiratory Infections (ARI) Control Programme and care of
the newborn.
3.5.89 These initiatives have resulted in a progressive decline in child mortality rates (Figure 14), IMR (Table 3.5.3), reduction in vaccine preventable diseases, mortality due to ARI and diarrhoeal disease. However, there are several lacunae both in the quality of care and coverage. The implementation of neonatal component is poor.
3.5.90 The fact that perinatal and neonatal mortality have not shown any substantial decline over the last two decades is a cause for concern. Improvement in the quality of antenatal, intranatal and neonatal care is urgently needed. Initiatives for detection and management of low birth weight babies, detection and management of birth asphyxia and essential newborn care have to be added in a phased manner to the existing package of services. The Child Health initiative during the Ninth Plan seeks to improve neonatal care through an "essential new born care package" so that reduction in neonatal mortality rate could be achieved. Improvement in the quality of services and coverage of ongoing Child health programmes will receive adequate attention. Child health care services will continue to include efforts for protection and promotion of breast feeding, advice for appropriately timed introduction of supplements to breastfed infants, improving utilisation of nutritional supplementation programmes under the ICDS, massive dose Vitamin A prophylaxis programme and anaemia prophylaxis programme.
3.5.91 The elimination of polio and neonatal tetanus and reduction in morbidity due to measles are possible and should be achieved within the Ninth Plan period. Efforts to improve ARI and Diarrhoeal Disease Control Programmes and effective management of infections will be the focus of child health services at primary health care level. These will result in a substantial reduction in IMR by 2002 AD. Linkages between primary, secondary and tertiary care institutions will enable rapid identification and effective management of complications of infectious diseases and non- communicable disease and reduce both death and disabilities.
3.5.92 There has been a substantial improvement in immunisation coverage over the last decade. The pulse polio campaign has shown that it is possible to effectively mobilise the service providers and the recipients and carry out a massive campaign successfully. Integrating these programmes into the Child Health programme over the next few years is essential for ensuring sustainability of these initiatives.
Male Participation in Planned Parenthood Movement
3.5.93 Men play an important role in determining education and employment status, age at marriage, family formation pattern, access to and utilisation of health and family welfare services for women and children. Their active co-operation is essential for the success of STD/RTI prevention and control. In condom users, consistent and correct use are essential pre-requisites for STD as well as pregnancy prevention. Vasectomy, which is safer and simpler than tubectomy, was widely accepted in the sixties. However, after 1977 there had been a steep and continuous decline in vasectomies (Figure 8). There is a need to find out and address the needs and conveniences of men seeking vasectomy and provide ready access to vasectomy services both in urban and rural areas. In institutions with adequate trained expert surgeons, `No-scalpel' vasectomy might provide a useful technique for popularisation of vasectomy among some segments of the population. During the Ninth Plan period due attention will be given to enhance men's participation in the Planned Parenthood movement.
Phasing of Reproductive Health Services
3.5.94 There are wide variations in the availability and utilisation of MCH and FP services between different States. During the Ninth Plan, district-specific approach aimed at achieving appropriate increment in the provision of services will be taken up so that there is improvement in maternal and child health status and acceptance of family planning methods in all districts and the gap between districts in terms of performance will diminish.
3.4.95 On the basis of their performance in the Family Welfare programme, as assessed by readily available data such as CBR, total fertility rate, IMR, female literacy, percentage registered for ANC, percentage of hospital deliveries, percentage of deliveries by trained personnel, the States/ districts may be classified into three groups - good, intermediate and poorly performing. Differential incremental additions to existing package of services will be provided in these three groups. In poorly performing States/ districts the major intervention will be to ensure hygienic, aseptic home-based deliveries by trained personnel, strengthening of sub-centres for providing immunisation and MCH services, improving services available at PHCs, strengthening selected PHCs, CHCs, District Hospitals and improving referral systems. In States/ districts in which majority of deliveries are already occurring in hospitals, attempts will be made towards ensuring 100% antenatal care and institutional deliveries. In addition, comprehensive reproductive health care services including prevention and management of RTI and STD and management of gynaecological problems will be made available in selected PHCs as well as CHCs. In States where already majority of women deliver in institutions, improvement in availability of MTP services in all PHCs/ CHCs, comprehensive reproductive and child health services and strengthening referral services will receive attention. In all States orientation training of all health workers in PHC-based planning and RCH care delivery will be carried out, so that they develop appropriate skills and learn to optimally utilise available facilities to provide adequate and appropriate health care to women and children in their area.
Reorganisation of Family Welfare Infrastructure
3.5.96 In the early 70s when the Family Welfare Programme was initiated, the infrastructure for providing MCH and Family Planning Services was non-existent at primary health care level, and sub-optimal in secondary and tertiary care levels. In order to quickly improve the situation, the Department of Family Welfare created and funded Post-partum Centres (A, B, and C types and subdistrict), urban Family Welfare Centres/ health post and provided additional staff to the then existing PHCs. In addition, the ANMs in the Sub-Centres, created after the initiation of the FW Programme, were also funded by the Department. The Department of Family Welfare also created State and district level infrastructure for carrying out the programmes and training institutions for pre/in-service training of personnel. All these activities are being funded through Plan funds of the Department of Family Welfare.
3.5.97 Over the last three decades family welfare services are being provided as an integral part of obstetric and gynaecological services by secondary and tertiary care institutions. So type A and B postpartum centres may be taken over by the State and merged with the Department of Obstetrics and Gynaecology in the respective hospitals during the Ninth Plan. The staff whose salaries are met from the head "Rural Family Welfare Centre" are functioning as Primary Health Centre officers in most States. The sub- district postpartum centre staff may be posted in FRUs. Over the next Plan period, these two categories of staff will become a part of State primary health care infrastructure.
3.5.98 It is imperative that the ANMs, who are crucial for increasing the outreach of the Programme, should be available and fully funded by the FW Programme. During the Ninth Plan, efforts will be made not only to fill the existing gaps in the manpower but also to provide additional ANMs on the basis of work load, difficulties in delivery of services and distances to be covered. This would ensure that the States do employ the required number of ANMs and achieve an improved outreach and better implementation of the Programme.
Strategies for Increasing Efficiency
3.5.99 A vast infrastructure for delivery of health and family welfare services has been created over the last three decades utilising uniform norms for the entire country. Though there has been a substantial improvement in the health and demographic indices the performance in some respects has been sub-optimal. There are marked differences in performance between the States; the States with poor demographic indices continue to remain poor performers in spite of special efforts to provide additional funding for manpower and infrastructure. Factors responsible for the sub-optimal performance include:
-
absence of proper medical hierarchy with well defined functions;
- lack of first line supervision and mechanism to bring about accountability;
- absence of referral system and lack of functional FRUs.
3.5.100 During the Ninth Plan, efforts will be made to improve efficiency by undertaking task analysis, assigning appropriate duties/ tasks to designated functionaries and training them to act as a multi-professional team. In such a command chain, the last link will be provided by the village-based workers who will act as a liaison person between the people and health functionaries and ensure utilisation of available facilities. The Panchayati Raj Institutions will participate in the planning and assist in the implementation and monitoring of the programme. The ANM will administer vaccines, screen infants, children and pregnant women, identify and refer the "at risk" persons to appropriate institution. The medical officer at PHC will undertake PHC-based planning and monitoring of the Health and Family Welfare programmes and provide curative services, organise and supervise preventive and promotive health and family welfare-related activities and develop a viable, functional referral systems. The specialists in CHC will provide appropriate emergency care and care for referred patients, participate in the development of the PHC based RCH programmes, monitor the activities and initiate midcourse corrections. If this pattern of functioning is followed, the community, the link worker and the health functionaries will be performing the tasks that they are best suited to do and the implementation of the programme will improve because of effective functioning.
Intersectoral Coordination
3.5.101 Effective implementation of Family Welfare Programme involves a great deal of inter-sectoral coordination. The related sectors have to take steps to enhance the status of women, particularly women’s literacy and employment, to raise age at marriage, their general development, generating more income in rural areas.
3.5.102 Concerned departments like Department of Women and Child Development, Human Resources Development, Agriculture, Rural Development, Urban Development, Labour, Railways, Industry need to :
-
involve their extension workers in propagating reproductive and child health care;
- include population stabilisation and RCH care in their curricula;
- use their own funds for improving awareness and access to family welfare services
3.5.103 The village-level functionaries - namely Anganwadi workers, Mahila Swasth Sangh (MSS), Traditional Birth Attendant (TBA), Krishi Vigyan Kendra (KVK) Volunteers, School teachers need to work together and achieve optimal utilisation of available services.
3.5.104 The opinion leaders at the national, State and local levels will participate in community education regarding the Family Welfare Programme so that community awareness and involvement vital to the success of this programme is improved. Simultaneously, the Ninth Plan will launch an intensive drive to promote health education so that India builds a sound foundation for a successful health programme. IEC on basic principles of hygiene, sanitation, nutrition, and prevention of illnesses and diseases will be promoted through not only the educational institutions and the adult education programme but also through the ICDS programme, the counselling offered by the health workers at all levels and the mass media.
Involvement of Non-Governmental Organisations (NGOs) and Voluntary Organisation for Promotion of Family Welfare
3.5.105 The Ministry of Health and Family Welfare has initiated several programmes involving NGOs in efforts to improve Family Welfare Programme. These include:
-
Revamping of Mini Family Welfare Centre in areas where the couple protection rates are below 35 percent;
-
Involvement of ISM and H practitioners;
-
Area-specific IEC activities through NGOs;
-
Establishment of Standing Committees for Voluntary Action (SCOVAs) to fund NGO projects promptly;
-
Identification of Government/ NGO organisations for training of NGOs in project formulation, programme management and monitoring.
-
These activities will be continued and intensified during the Ninth Plan period.
Private Sector Participation in RCH
3.5.106 It is estimated that the private sector accounts for more than three quarters of all health care expenditure in India. Private sector provides MCH and family planning services also but to a lesser extent. It is increasingly recognised that the private sector represents an untapped potential for increasing the coverage and improving the quality of reproductive and child health services in the country. The challenge is to find ways and means to optimally utilise their potential. The major limitations in the private sector include the following:
-
the focus has till now been mainly on curative services;
- the quality of services is often variable;
- as the users have to pay for the services the poorer sections of population cannot afford these services.
3.5.107 Some of the initiatives could be through collaboration between public and private sector in providing health care to the poorer segments of population who cannot afford to pay for health services. While organising the involvement of private medical practitioners in RCH care, it is essential to provide orientation training to all and ensure utilisation of their services in a cost-effective and sustainable basis.
3.5.108 Private/ voluntary organisations providing health care to women are relatively small in number but they could play an effective role in the delivery of reproductive and child health care services at affordable cost, especially in certain specific locations such as urban slums. Giving the private sector and voluntary organisations appropriate incentives to broaden the range of activities and improve the quality of reproductive and child health-related services they offer are other avenues that require exploration. Continued collaboration, training and technical assistance by governmental agencies to private medical practitioners and private/ voluntary organisations may help in strengthening reproductive and child health services in remote or under-served areas.
3.5.109 The NDC Committee on Population had recommended that managerial capability of the corporate bodies need to be harnessed for improving the social marketing of contraceptives, streamlining of health services and improving material and manpower management. The problem-solving approach of the corporate sector can be of use in improving the operational efficiency of the health care infrastructure. The corporate sector could participate in the delivery of primary health and family welfare care in the vicinity of their factories. They could provide tertiary care in collaboration with the Government sector institutions. During the Ninth Plan, the participation of the organised and unorganised sectors of industry, trade/ labour unions and agriculturists in family welfare programme will be further strengthened.
Research and Development
3.5.110 The ICMR is the nodal research agency for funding basic, clinical and operational research in contraception and MCH. In addition to ICMR, CSIR, DBT and DST are some of the major agencies funding research pertaining to Family Welfare Programme.
|
Research and Development Basic and Clinical Research Development and testing of new contraceptives including contraceptives which are considered to be effective in Indian Systems of Medicine Research on methods for male fertility regulation Clinical trials on newer non-surgical methods of MTP Post-marketing surveillance of Centchroman. Operational Research
|
The National Committee for Research in Human Reproduction assists the Department of Family Welfare in drawing up priority areas of research and ensuring that there is no unnecessary duplication of research activities. Some of the major institutions carrying out research in this area include the Institute for Research in Reproduction , Bombay, National Institute of Nutrition, Hyderabad, National Institute of Health and Family Welfare, New Delhi, Central Drug Research Institute, Lucknow and the Central Council for Research in Ayurveda and Siddha, Delhi. A network of 18 Population Research Centres conduct studies on different aspects of the Family Welfare Programme and undertake demographic surveys.
3.5.111 Basic research efforts for the development of newer technology for contraceptive drugs and devices currently under way are unlikely to lead to availability of newer methods for use in the programme during the next decade. These efforts are needed to cater to the requirements of the population in the decades to follow. For improving the contraceptive coverage for men and women, efforts need to be directed towards improving the quality of care and assist men and women to choose appropriate contraceptives from those currently available. Therefore, the emphasis must be on operational research for improving the performance of Family Welfare Programme and socio-behavioural research to improve community participation for increased acceptance of family welfare services. It is important that an appropriate institutional mechanism is created and supported to test and ensure the quality control in products utilised in the programme.
Basic and Clinical Research
3.5.112 Basic and clinical research studies in the priority areas identified earlier will be continued during the Ninth Plan period. These include development and testing of:
-
Drug delivery systems for the delivery of contraceptive steroids;
- Vaso-occlusive methods;
- Spermicides based on plant products such as neem oil and saponins and
- Vaginal contraceptives including those using plant based substances.
- Testing contraceptives, which are considered to be effective in Indian Systems of Medicine and/or used among tribals.
- Research on methods for male fertility regulation including long-acting androgens.
- Clinical trials on newer non-surgical methods of MTP.
- Post-marketing surveillance for Centchroman.
Operational Research
3.5.113 During the last year of the Eighth Plan the Department of Family Welfare has changed over to decentralised PHC based area-specific micro planning and implementation of Reproductive and Child Health Care. Due to problems inherent in such a massive shift, there had been a discernible decline in performance in terms of contraceptive acceptance in most of the States. In order to rapidly reverse this trend it is imperative that all service providers, in the Government, voluntary and private sector are trained so that they understand and implement the programme and the population understands and appropriately utilises the available facilities. In order to rapidly translate the written guidelines to actual implementation and remove operational obstacles it is imperative that operational research studies on a massive scale are taken up in different settings in the States.
3.5.114 Studies on the ongoing demographic transition and its consequences will be encouraged. Studies on continuation rates and use effectiveness of contraceptives under the programme conditions will be undertaken so that these could be used for computing effective couple protection rates.
3.5.115 The term `operational research' has been used to cover a wide variety of formal research studies of varying scale carried out by research workers belonging to different disciplines. In addition to strengthening these types of formal research studies, it might become necessary to encourage the local population, health service providers and others who want to try innovative methods to tackle the local problems. Research is also required in operationalising integrated delivery of RCH services, nutrition, education, women and child development, rural development and family welfare services at the village level, utilising the available infrastructure under various programmes.
Monitoring of Family Welfare Services
3.5.116 Monitoring and evaluation form an essential component of FW Programme. Indicators used for monitoring and evaluation include process indicators and impact indicators. Process indicators are used to monitor the progress of implementation of the programme through monthly progress reports as compared to the annual targets/ Expected Level of Achievements (ELAs). The existing service statistics do provide an inbuilt rapid and ready method for assessment of performance in Family Welfare Programme in terms of process indicators eg., Table 3.5.8 for ANC and Table 3.5.6 for immunisation and FP acceptance. These data are used for mid-course corrections in the States that are not achieving the expected level of performance. However, these indicators do not provide any information on the quality of care or appropriateness of the services. In the Ninth Plan period, the programme will also monitor a set of `quality of care' indicators. During the Ninth Plan, efforts will be made to collate and analyse service data collected at the district level and respond rapidly to the evolving situations. Available data from census, demographic and health surveys undertaken in the district by various agencies including the Population Research Centres will be analysed and utilised at the local level for area-specific micro planing. Efforts will be made to incorporate the district-level information from other sectors and optimally utilise the local resources including human resources in the implementation of the Family Welfare Programme, through inter-sectoral coordination. Efforts will also be made to generate district- level data on all the related sectors and utilise them for programme planning , monitoring and evaluation.
3.5.117 The Department of Family Welfare has constituted regional evaluation teams which carry out regular verifications and validate the acceptance of various contraceptives. During the Ninth Plan period these evaluation teams will be used to obtain vital data on failure rates, continuation rates and complications associated with different family planning methods.
3.5.118 The Office of the Registrar General of India (RGI) works out the annual estimates of crude birth rate, crude death rate and infant mortality rate through their scheme of Sample Registration System. The system provides an independent evaluation of the impact of the Family Welfare Programme in the country. The vital indices and decennial growth rate estimated by the Office of the Registrar General of India on the basis of the census also provides indirect evaluation of impact of the Family Welfare programme.
3.5.119 Available information with RGIs office indicates that as of mid-nineties over 90% of all births and deaths are registered in states like Kerala, Tamil Nadu, Delhi, Punjab and Gujarat. In these States these data will be used at district-level both for PHC-based planning of RCH care as well as evaluation of the RCH care annually. In districts where vital registration is over 70%, efforts will be stepped up to ensure that over 90% of births and deaths are reported so that independent data base is available for planning as well as impact evaluation of PHC- based RCH care. The Department of Family Welfare, in collaboration with RGI, has set a target of 100% registration of births and deaths by the end of the Ninth Plan. Steps to collect, collate and report these data at PHC/District level on a yearly basis have also been initiated.
Expected Levels of Achievement (ELA) for the Ninth Plan
3.5.120 The performance under the Family Welfare Programme will depend upon
-
Programme initiatives during the Ninth Plan;
- Financial resources available;
- Capability and effectiveness of the infrastructure and manpower to carry out the programme;
- Literacy and economic status of the families particularly of the women;
- Policy support by opinion leaders and the society.
3.5.121 During the Ninth Plan, the FW Programme will attempt to meet the unmet need for family planning and provide MCH services so that there is a substantial reduction in IMR and under `five' mortality rate. In view of the marked differences in the availability and utilisation of family welfare services and IMR CBR and CPR between States, a differential approach to the implementation of Family Welfare Programme is necessary. Consequently, during the Ninth Plan period the ELA in terms of process and impact indicators will be State specific.
3.5.122 Any projection of expected levels of achievement for process and impact indicators at the end of the Ninth Plan has to take into consideration the pace of improvement in these indicators during the Eighth Plan and the additional policy and programme measures envisaged to accelerate the pace of achievement during the Ninth Plan. The State- specific projections have been worked out at two different levels of achievement, one on the basis of the assumption that the trend observed with regard to these parameters in the last 15 years will continue during the Ninth Plan period and the second on the assumption that the additional policy and programme initiatives provided during the Ninth Plan period will result in the acceleration of the pace and result in more substantial improvement during the Ninth Plan period. The expected levels of achievement under both these assumptions have been computed State wise and are given in Table 3.5.10 and 11.
3.5.123 The expected levels of achievement by the terminal year of Ninth Plan (2002) are given below:
|
Indicator |
If current trend continues |
If acceleration envisaged in Approach Paper to the Ninth Five Year Plan is achieved |
|
C B R |
24/1000 |
23/1000 |
|
I M R |
56/1000 |
50/1000 |
|
T F R |
2.9 |
2.6 |
|
C P R |
51% |
60% |
|
NNM R |
35/1000 |
|
|
M M R |
3/1000 |
National Population Policy
3.5.124 Population and sustainable development are key issues that have determined the improvement in quality of life over the last five decades. There have been massive changes in demographic and health indices of the population. India is currently in the midst of demographic transition. The next two decades will witness an unprecedented increase in the number of persons in 15-59 age group and there is a need to meet health and contraceptive needs of this population. The number of births may remain unaltered but there is an urgent need to reduce maternal and infant mortality so that there is a reduction in the desired level of fertility.
3.5.125 There has been a paradigm shift in Family Welfare Programme; centrally defined method specific targets have been replaced by community based need assessment and decentralised planning and implementation of the programme to fulfil these needs. The ongoing educational, info-technology and socio-economic transition have raised awareness and expectations of the population. Taking all these into account it is imperative that a National Population Policy is drawn up so that it provides reliable and relevant policy frame work not only for improving Family Welfare Services but also for measuring and monitoring the delivery of family welfare services and demographic impact in the new millenium.
Funding for Family Welfare Programme
3.5.126 The National Family Welfare Programme is a 100% Centrally funded scheme. Even after twenty five years of initiation of Family Welfare Programme, the Department meets the cost of maintenance of infrastructure, manpower, consumables and other costs for provision of family welfare services from central Plan funds. The outlays and expenditure for Family Welfare Programme during different Plan periods are shown in Table 3.5.7. Allocations for Family Welfare ranged between 1.1 to 1.8% of total Plan outlays. Eighth Plan outlays and expenditure is shown in Table 3.5.12. Right from the first year of the Eighth Plan, the expenditure of the Department has been higher than the outlay provided for each year of the plan. In addition the Department has to reimburse the states for expenditure incurred as arrears.
3.5.127 More than 75% of the expenditure on the programme is committed expenditure being incurred towards staff salaries and maintenance of infrastructure. There are problems in continued plan funding of non-plan activities under the Family Welfare Programme, but keeping in view the importance of achieving sustainable population growth rate, the National Family Welfare Programme will continue to be centrally sponsored programme and all expenditure will continue to be made from the plan outlay of the Department of Family Welfare during the Ninth Plan.
3.5.128 It is imperative that the ANMs, who are crucial for the outreach of the Programme should be available and her salary fully met Family Welfare Programme. During the Ninth Plan efforts will be made not only to fill the existing gaps in the manpower but also to provide additional ANMs on the basis of workload, difficulties in delivery of services and distances to be covered. The Department of Family Welfare provides funds for the maintenance of 97,757 sub-centres out of 1,36,339 functioning sub-centres. Planning Commission had repeatedly emphasised the need for financing all the functioning sub-centres so that the ANMs who are crucial peripheral workers for implementation of the Family Welfare Programme are in position at all the sub-centres.
3.5.129 The Department of Family Welfare bears the costs of maintenance of rural family welfare subcentres, post-partum centres, urban family welfare services and training activities according to certain norms which were fixed long back. There is a wide gap between the actual funds required to maintain the above services and the funds being provided according to the norms. Thus, it results in the accumulation of arrears payable to the states. The delay in the payment of arrears to the states affects provision of family welfare services in the states whose financial position is not very good. This is especially true for the states like Bihar, U.P etc which are weak in terms of demographic indicators. Thus, there is an urgent need to review the norms for providing funds to the states for implementation of the Family Welfare Programmes. The Department of Family Welfare has already constituted a committee to review these norms. During the Ninth Five Year Plan adequate financing should be made to the states so that the programme activities are implemented without generation of any arrears.
3.5.130 The Department of Family Welfare has initiated multi-agency externally funded project "Reproductive and Child Health Care" from the year 1996-97. The project will promote effective maternal care to ensure safe motherhood, increased access to contraceptive care, prevention and treatment of RTI/STD, reproductive health care services for adolescents etc. The total cost of the project which is to be implemented during the Ninth Plan period is Rs. 5112 crores out of which Rs.3600 crores is expected to be the external assistance and the balance amount is to be provided by the Government of India for sustaining the on-going maternal and child health care activities and for counter part funding for the RCH Project. It is, therefore, imperative that sufficient funds are provided to the Department of Family Welfare so that the department is able to absorb to external funding under the project during the Ninth Plan period.
3.5.131 During the Eighth Plan period the Central departments like Railways, Post and Telecommunications, have internalised the expenditure on family welfare services to their employees. Family welfare services are part of the welfare services like health care, pension, gratuity etc. extended to the employees by their respective departments. All departments, both of Central and State Governments, public sector undertakings and autonomous bodies etc., should be persuaded during the Ninth Plan to internalise the family welfare expenditure within their respective budgets. The modalities for such a shift have to be worked out by the concerned State and Central Departments, the Finance Ministry and the Planning Commission.
3.5.132 In view of the importance of IEC campaign in improving utilisation of available services for RCH care, Doordarshan and Akashvani will be persuaded to provide specific time slots on a larger scale either free or on concessional rates for IEC efforts.
3.5.133 Over the last 40 years there has been considerable escalation in the cost of drugs. Supply of adequate quantities of drugs, vaccines and contraceptives is an essential pre-requisite for ensuring adequate coverage. In the Eighth Plan period there has been adequate supply of vaccine for pregnant women and vaccines to be given to infants. Contraceptive supplies have by and large been adequate. However, there have been a substantial shortfall in the supply of IFA and Vitamin A for achieving 100% coverage of the target groups. It is imperative that the drugs, vaccines and contraceptives to completely cover all the target groups on the basis of the projected population is provided (Table 3.5.13). Adequate funding for purchase of these needs to be made available so that coverage will improve. It is essential that the supply of these items are continued and provided free of charge to all segments of population because even among the population above the poverty line, there is often considerable reluctance to meet the expenses for women and children especially for preventive programmes. The services and supplies under Family Welfare Programme should continue to be provided free of cost so that inability to pay for preventive and promotive services does not become a barrier to the acceptance of Family Welfare Programme and the achievement of the desired family size. Taking all the above factors into consideration, the Department of Family Welfare has been provided with an outlay of Rs. 15120.20 crores for the Ninth Plan period. The outlay for Annual Plans will be adjusted depending upon the requirements of the department and availability of funds including reimbursement from EAPs.
<<Previous