3.5 FAMILY WELFARE
Introduction
 3.5.1
Human development is the ultimate objective of all planning efforts.
Planning takes into account the resources and pathways available for
human development and human resources available for carrying out the
developmental Plans. India, the second most populous country in the
world, has no more than 2.5% of global land but is the home of 1/6th
of the world's population. The prevailing high maternal, infant, childhood
morbidity and mortality, low life expectancy and high fertility and
associated high morbidity had been a source of concern for public health
professionals right from the pre-independance period. The Bhore Committee
Report (1946) which laid the foundation for health service planning
in India, gave high priority to provision of maternal and child health
services and improving their nutritional and health status. It is noteworthy
that this report which emphasized the importance of providing integrated
preventive, promotive and curative primary health care services preceded
the Alma Ata declaration by over three decades. Under the Constitution
of India elimination of poverty, ignorance and ill health are three
important goals. Successive Five Year Plans have been providing the
policy frame work and funding for planned development of nationwide
health care infrastructure, manpower, drugs, devices and other essential
items for improving health status of mothers and their children needed
for improving health status of women and children and to meet all the
felt needs for fertility regulation.
3.5.1
Human development is the ultimate objective of all planning efforts.
Planning takes into account the resources and pathways available for
human development and human resources available for carrying out the
developmental Plans. India, the second most populous country in the
world, has no more than 2.5% of global land but is the home of 1/6th
of the world's population. The prevailing high maternal, infant, childhood
morbidity and mortality, low life expectancy and high fertility and
associated high morbidity had been a source of concern for public health
professionals right from the pre-independance period. The Bhore Committee
Report (1946) which laid the foundation for health service planning
in India, gave high priority to provision of maternal and child health
services and improving their nutritional and health status. It is noteworthy
that this report which emphasized the importance of providing integrated
preventive, promotive and curative primary health care services preceded
the Alma Ata declaration by over three decades. Under the Constitution
of India elimination of poverty, ignorance and ill health are three
important goals. Successive Five Year Plans have been providing the
policy frame work and funding for planned development of nationwide
health care infrastructure, manpower, drugs, devices and other essential
items for improving health status of mothers and their children needed
for improving health status of women and children and to meet all the
felt needs for fertility regulation.
 3.5.2
In 1951, the infant republic took stock of the existing situation in
the country and initiated the first Five Year Development Plan. Living
in a resource poor country with high population density, the Planners
recognised in the census figures of 1951, the potential threat posed
by population explosion and the need to take steps to avert it. It was
recognised that population stabilisation is an essential prerequisite
for sustainability of development process so that the benefits of economic
development result in enhancement of the well being of the people and
improvement in quality of life. India became the first country in the
world to formulate a National Family Planning Programme in 1952, with
the objective of "reducing birth rate to the extent necessary to
stabilise the population at a level consistent with requirement of national
economy". Thus, the key elements of health care to women and children
and provision of contraceptive services have been the focus of India’s
health services right from the time of India’s independence. Successive
FiveYear Plans have been providing the policy framework and funding
for planned development of nationwide health care infrastructure and
manpower. The Centrally Sponsored and 100% centrally funded Family Welfare
Programme provides additional infrastructure, manpower and consumables
needed for improving health status of women and children and to meet
all the felt needs for fertility regulation.
3.5.2
In 1951, the infant republic took stock of the existing situation in
the country and initiated the first Five Year Development Plan. Living
in a resource poor country with high population density, the Planners
recognised in the census figures of 1951, the potential threat posed
by population explosion and the need to take steps to avert it. It was
recognised that population stabilisation is an essential prerequisite
for sustainability of development process so that the benefits of economic
development result in enhancement of the well being of the people and
improvement in quality of life. India became the first country in the
world to formulate a National Family Planning Programme in 1952, with
the objective of "reducing birth rate to the extent necessary to
stabilise the population at a level consistent with requirement of national
economy". Thus, the key elements of health care to women and children
and provision of contraceptive services have been the focus of India’s
health services right from the time of India’s independence. Successive
FiveYear Plans have been providing the policy framework and funding
for planned development of nationwide health care infrastructure and
manpower. The Centrally Sponsored and 100% centrally funded Family Welfare
Programme provides additional infrastructure, manpower and consumables
needed for improving health status of women and children and to meet
all the felt needs for fertility regulation.
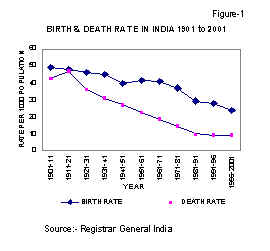
 3.5.3
The technological advances and improved quality and coverage of health
care resulted in a rapid fall in Crude Death Rate (CDR) from 25.1 in
1951 to 9.8 in 1991. In contrast, the reduction in Crude Birth Rate
(CBR) has been less steep, declining from 40.8 in 1951 to 29.5 in 1991.
As a result, the annual exponential population growth rate has been
over 2% in the last three decades. During the Eighth Plan period the
decline in CBR has been steeper than that in the (CDR) and consequently,
the annual population growth rate has been around 1.9% during 1991-95.
(Figures 1 and 2). The rate of decline in population growth is likely
to be further accelerated during the Ninth Plan period.
3.5.3
The technological advances and improved quality and coverage of health
care resulted in a rapid fall in Crude Death Rate (CDR) from 25.1 in
1951 to 9.8 in 1991. In contrast, the reduction in Crude Birth Rate
(CBR) has been less steep, declining from 40.8 in 1951 to 29.5 in 1991.
As a result, the annual exponential population growth rate has been
over 2% in the last three decades. During the Eighth Plan period the
decline in CBR has been steeper than that in the (CDR) and consequently,
the annual population growth rate has been around 1.9% during 1991-95.
(Figures 1 and 2). The rate of decline in population growth is likely
to be further accelerated during the Ninth Plan period.  Though
the decline in CBR and CDR has occurred in all States, the rate of decline
in CBR was slower in some States like U.P. and Bihar (Table-3.5.1).
There are substantial differences in CBR and IMR between States (Figure
3 and 4) and even within the same State there are substantial differences
between districts. The efforts of the Family Welfare Programme during
the Ninth Plan will be to minimise the existing disparities by providing
resources to fill the crucial gaps in infrastructure and manpower in
primary health care in both urban and rural areas and improving the
operational efficiency of health system. The emphasis on improving the
access and quality of reproductive and child health services will enable
the increasingly aware and literate families to attain their reproductive
goals in harmony with the national goals.
Though
the decline in CBR and CDR has occurred in all States, the rate of decline
in CBR was slower in some States like U.P. and Bihar (Table-3.5.1).
There are substantial differences in CBR and IMR between States (Figure
3 and 4) and even within the same State there are substantial differences
between districts. The efforts of the Family Welfare Programme during
the Ninth Plan will be to minimise the existing disparities by providing
resources to fill the crucial gaps in infrastructure and manpower in
primary health care in both urban and rural areas and improving the
operational efficiency of health system. The emphasis on improving the
access and quality of reproductive and child health services will enable
the increasingly aware and literate families to attain their reproductive
goals in harmony with the national goals.
Approach during the Ninth Plan
3.5.4 Reduction in the population growth rate has been recognised as one of the priority objectives during the Ninth Plan period. The current high population growth rate is due to: (1) the large size of the population in the reproductive age-group (estimated contribution 60%); (2) higher fertility due to unmet need for contraception (estimated contribution 20%); and (3) high wanted fertility due to prevailing high IMR (estimated contribution about 20%).
3.5.5 While the population growth contributed by the large population in the reproductive age group will continue in the foreseeable future, the other two factors need effective and prompt remedial action.
|
The objectives during the Ninth Plan will be:
The strategies during the Ninth Plan will be:
|
3.5.6 The enabling objectives during the Ninth Plan period, therefore, will be to reduce the population growth rate by
- meeting all the felt-needs for contraception; and
- reducing the infant and maternal morbidity and mortality so that there is a reduction in the desired level of fertility
The strategies during the Ninth Plan will be:
-
To assess the needs for reproductive and child health at PHC level and undertake area- specific micro planning; and
-
To provide need-based, demand-driven high quality, integrated reproductive and child health care.
-
Bridging the gaps in essential infrastructure and manpower through a flexible approach and improving operational efficiency through investment in social, behavioural and operational research
- Providing additional assistance to poorly performing districts identified on the basis of the 1991 census to fill existing gaps in infrastructure and manpower.
- Ensuring uninterrupted supply of essential drugs, vaccines and contraceptives, adequate in quantity and appropriate in quality.
- Promoting male participation in the Planned Parenthood movement and increasing the level of acceptance of vasectomy.
3.5.7 Efforts will be intensified to enhance the quality and coverage of family welfare services through:
- Increasing participation of general medical practitioners working in voluntary, private, joint sectors and the active cooperation of practitioners of ISM and H;
- Involvement of the Panchayati Raj Institutions for ensuring inter-sectoral coordination and community participation in planning, monitoring and management;
- Involvement of the industries, organised and unorganised sectors, agriculture workers and labour representatives.
Evolution of India’s Family Welfare Programme
The fifties
3.5.8 At the time of Independence the health care services in India were predominantly urban, hospital based and curative. General practitioners well versed in maternal child health and paediatricians and obstetricians provided health care to women and children who came to them. They did provide comprehensive, integrated, good quality services but technology available for detection and management of health problems was limited and out reach of services was poor. Majority of the population especially those belonging to the poorer segment and those residing in rural areas did not have access to health care. Consequently the morbidity and morality rates in them was quite high. Many women died while seeking illegal induced abortion to get rid of unwanted pregnancy because they did not have access to contraceptive care for preventing pregnancies. Conceptions that were too early, too close, too many and too late resulted in high maternal and infant mortality rates. Antenatal, intrapartum, postnatal and contraceptive care were not readily available to women who required these services desperately.
3.5.9 Obstetricians, who were daily witnessing maternal morbidity and mortality associated with high parity, were ready and willing to persuade their patients who had completed their families, to undergo surgical sterilisation. The fact that the technique was simple, safe and effective and could be done soon after delivery under local anaesthesia, accounted for the popularity of postpartum tubal sterilisation. The safety, simplicity and efficacy of vasectomy was also well recognised. For a couple who had completed their family, sterilisation of one partner resulted in the reduction of maternal morbidity and mortality associated with high parity. To some extent this was responsible for the substantial drop in maternal mortality rates observed in the urban areas during the 1950s. However, these measures had no impact on the fertility rate or the population growth rate of the country because of poor outreach to rural population. Thus in fifties good quality integrated maternal and child health care, and family planning services were available to those who were aware, had access and could afford the services of the physicians. There were efforts to improve the coverage of the population and extend the services to rural areas as a part of the block development programme; resource and manpower constraints were responsible for the slow progress in this effort.
The sixties
3.5.10 The sixties witnessed a seachange with availability of safe effective vaccines for many communicable diseases, and effective contraceptives such as Lippe’s loop for prevention of pregnancy; programmes for providing these to the population as well as programmes for improvement of nutritional status of vulnerable groups were initiated during this period. In order to reach the benefits of the technological innovations to the population, certain identified priority interventions were implemented by a well knit team of professionals who looked after the programme requirements and implementation at the periphery was done through the limited health care infrastructure available in rural areas. The Family Planning and the immunisation programme were among the earliest of such programmes; subsequently several other vertical programmes were added. In an attempt to improve the out reach, camp approach was taken up for providing care to pregnant women and children; these efforts however did not result in any marked improvement in health status of these vulnerable groups because the care was not available when needed and referral services were not available.
3.5.11 Rapid growth of the population in the previous 10 years, reported in the 1961 census, stimulated the Government to form a Department of Family Planning, with a modest budget. The health infrastructure was still predominantly urban based. During the 1960s, sterilisation remained the focus of the National Family Planning Programme. Efforts were made to popularise vasectomy and to provide vasectomy services to rural areas, using a camp approach. Tubectomy services, however, remained based predominantly in urban hospitals. Extension education approach to improve awareness and increase acceptance of F.P. methods were also included. Lippe’s loop provided the first reliable birth spacing method for women in India. Following encouraging response in urban clinic attempts were made to provide this spacing method to the rural population through camp approach. However, without infrastructure to provide the follow up services the device fell into disrepute. It was obvious that without substantial inputs into infrastructure and manpower to provide the needed follow up services it will not be possible to achieve any substantial improvement in Maternal and Child Health indices or reduce birth rates.
Seventies
3.5.12 The seventies witnessed many initiatives to improve the health and nutritional status of women and children. The massive dose Vit.A programme aimed at prevention of nutritional blindness, the anaemia prophylaxis programme aimed at reducing anaemia and associated ill health and food supplementation to pregnant and lactating women and children below five years through ICDS were major initiatives to tackle under nutrition and its adverse consequences in women and children. With the improvement in primary health care infrastructure access to health care improved.
3.5.13 The census of 1971 showed that population explosion was no longer a potential threat but a major problem to be tackled. The government gave top priority to the Family Planning programme and provided substantial funds for several new initiatives. Sterilisation, IUD and condoms were made available through the Primary Health Centres. The hospital based Postpartum Progamme provided contraceptive care to women coming for delivery. The MTP act enabled women with unwanted pregnancy to seek and obtain safe abortion services.
3.5.14 Increasing concern about rapidly growing population led to the Family Planning Programme being included as a priority sector programme during the Fifth Plan. The massive sterilisation drive of 1976 did result in eight million persons undergoing sterilisation, but this did not have any perceptible impact on the birth rate as the cases were not appropriately chosen. The very next year showed a steep fall in the acceptance. In 1979 the Programme was renamed as Family Welfare Programme; increasing integration of family planning services with those of MCH and Nutrition was attempted.
Eighties
3.5.15 In 1983 India formulated the National Health Policy, which provided comprehensive frame work for planning, implementation and monitoring of Health care services. The National Health Policy:
- Reviewed the progress achieved in the delivery of health services
- Provided a situation analysis of the progress achieved in health, family welfare and nutrition programmes
- Identified priority areas for intervention in the next two decades
- Defined the policy, strategy and programme intervention in these priority areas
- Set the goals to be achieved by 2000 AD
3.5.16 Subsequent Plans have attempted to evolve and implement intervention Programmes to achieve the goals set in the National Health Policy.
3.5.17 A major initiative was taken during the Seventh Plan to provide facilities/services nearer to the doorsteps of population. The primary health care infrastructure was expanded:
- It was envisaged to have one sub-centre for every 5000 population in plain areas and for 3000 population in hilly and tribal areas. At the end of Seventh Plan i.e. 31.3.90, 1.30 lakhs sub-centres were established in the country.
- The Post Partum Programme was progressively extended to sub-district level hospitals. At the end of the Seventh Plan 1075 sub district level hospitals and 936 health Posts were sanctioned in the country, out of which the number functioning were 1012 and 870 respectively.
- The Universal Immunization Programme, started in 30 Districts in 1985-86, was extended to cover 448 districts in the country by the end of the Seventh Plan.
- Urban family welfare outposts and centres were established to provide improved access to family welfare services to the vulnerable slum population.
3.5.18 Focussed attempts were made to improve the immunisation coverage through Universal Immunisation Programme (UIP) mission mode project. Attempts were also made to improve antenatal coverage, improve the coverage under ORT and ARI Programme.
Eighth Plan Initiatives
3.5.19 Containing population growth was one of the six major objectives of the Eighth Plan. Recognizing the fact that reduction in infant and child mortality is an essential pre-requisite for acceptance of small family norm, Government of India has attempted to integrate MCH and Family Planning as part of Family Welfare services at all levels. NDC approved modified Gadgil Mukherjee Formula which for the first time gave equal weightage to performance in MCH Sector (IMR reduction) and FP Sector (CBR reduction) as a part basis for computing central assistance to non special category States. This initiative ensured that the inter linkages between Family Welfare Programme and Development was kept in focus in State Plans.
3.5.20 In order to give a new thrust and dynamism to the ongoing Family Welfare Programme the National Development Council set up a Sub-Committee on Population to consider the problem of population stabilisation and come up with recommendations to improve performance. The report of the sub-committee was considered and the recommendations were endorsed by the NDC in its meeting in September 1993. The NDC Committee on Population had recommended that Family Welfare Programme should take cognizance of the area specific socioeconomic, demographic and health care availability differentials and allow requisite flexibility in programme planning and implementation. For this purpose the NDC Committee recommended that there should be
|
The NDC Committee on Population has recommended that there should be:
Creation of district level databases on quality and coverage and impact indicators for monitoring the programme ICPD has advocated similar approach. Concordance between National (NDC Committee) and International (ICPD) efforts has improved funding and accelerated the pace of implemention of the family welfare programme. |
- Decentralised area specific planning based on the need assessment
- Emphasis on improved access and quality of services to women and children
- Providing special assistance to poorly performing states/districts to minimise the inter and intra-state differences in performance
- Creation of district level databases on quality and coverage and impact indicators for monitoring the programme.
3.5.21 The Department of Family Welfare started implementing the recommendations of the NDC Committee on Population during the Eighth Plan period. Funds from Social Safety Net (SSN) Programme were earmarked for improving primary health care infrastructure in poorly performing districts identified on the basis of IMR and CBR of 1981 census estimates. Implementation of Child Survival and Safe Motherhood (CSSM) Programme was initiated in the very first year of the Eighth Plan in these districts. A project to revitalise the Family Welfare Programme in Uttar Pradesh was taken up with external assistance.
3.5.22 The Child Survival and Safe Motherhood Programme (CSSM) was initiated in 1992. Under the Programme efforts were made to provide integrated antenatal, intranatal and postnatal care to women; the child health care component included immunisation, diarrhoeal and acute respiratory infection prevention and management programmes. The pulse polio initiative aimed at eradication of polio by 2000 AD was initiated in 1996.
3.5.23 In response to the recommendations of the NDC that there should be decentralised area specific need assessment and microplanning to meet the local needs, the department abolished the centrally defined method specific targets for family planning planning in two states (Tamil Nadu and Kerala) and 18 districts in 1995-96. Encouraged by the response in these two states, Department of Family Welfare has abolished the method specific centrally defined targets throughout the country and changed over to PHC based community need assessment, planning and implementation of Family Welfare Programme. Efforts are underway to improve access and quality of care to women and children.
3.5.24 The International Conference on Population and Development (ICPD) was held in Cairo in 1994. Major recommendations of the ICPD include:
-
Holistic reproductive health care should be made available through primary health care system.
- Efforts should be made by all the states to reduce infant mortality by one-third and maternal mortality by 50% by 2000 AD.
- Need assessment and need fulfillment as key elements for improving reproductive health.
3.5.25 India is a signatory to the ICPD; the recommendations of the ICPD are essentially similar to the recommendations of the NDC Committee on Population. The concordance between the National and International efforts has enabled the programme to get all the necessary political, economic and administrative support and gain further momentum to enable the individual and the country to fulfill their felt needs in reproductive health.
|
Major Achievements of FW Programme are:
Increase in Couple Protection Rate (CPR) from 10.4% (1970-71) to 45.4% (31.3.1997). |
Achievements of the Family Welfare Programme:
 3.5.26
As a part of the Plan exercise the Planning Commission and the Department
of Family Welfare have been laying down targets for health and family
welfare activities and for demographic indicators. Over the years, there
has been a progressive improvement in the achievement of most of these,
because the targets set were realistic and necessary inputs were provided
for their achievement. The targets and achievements in the different
Plan periods are given in Table 3.5.2.
3.5.26
As a part of the Plan exercise the Planning Commission and the Department
of Family Welfare have been laying down targets for health and family
welfare activities and for demographic indicators. Over the years, there
has been a progressive improvement in the achievement of most of these,
because the targets set were realistic and necessary inputs were provided
for their achievement. The targets and achievements in the different
Plan periods are given in Table 3.5.2.
3.5.27 The major achievements of the FW Programme are given in Table 3.5.3.
These include:
-
Reduction in Crude Birth Rate (CBR) from 40.8 (1951 Census) to 27.4 in 1996 (SRS 96)
- Reduction in Infant Mortality Rate (IMR) from 146 in 1951 to 72 in 1996 (SRS),
- Increase in Couple Protection Rate (CPR) from 10.4% (1970-71) to 45.4% (31.3.1997).
The
National Family Health Survey 1992-93 showed that :
11.0% for birth spacing methods and 8.5% for terminal methods |
The couple protection rate achieved and the birth rates since 1971 are summarised in Figure 5.
3.5.28 During the initial fifteen years (1971-85) there was a relatively steep increase in the couple protection rates. The reduction in the CBR was however not commensurate with the increase in couple protection rates. In the last ten years, the rise in CPR is less steep, but the fall in CBR has been steeper than in the earlier years.
3.5.29
The relationship between couple protection rates and CBR is complex.
There is a time lag of one to two years before the impact of contraceptive
acceptance is visible by way of reduction in birth rate. The age and
parity of the acceptors of contraception, and the continuation rates
of temporary methods of contraception are some of the existing factors
that determine birth rates. The trends in CPR and CBR over the last
25 years suggest that over the years there has been an improvement in
the acceptance of appropriate contraception at appropriate time. During
the Ninth Plan the FW Programme will focus its attention on need assessment,
counselling, provision of appropriate contraceptive and good follow
up services. Ensuring effective implementation of the FW programme will
result in a substantial improvement in CPR and reduction in CBR. 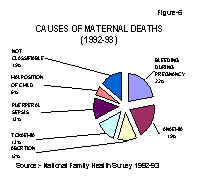
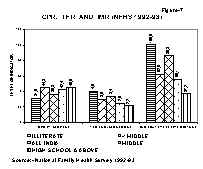
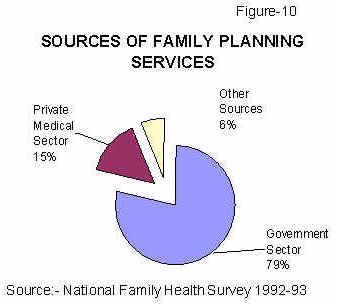
3.5.30 The National Family Health Survey indicated that in 1992-93: (a) 40.6% of currently married women used contraceptives; b) awareness about contraception was universal indicating that the IEC efforts in this direction had succeeded in reaching the population; c) in all States the wanted fertility was lower than the actual fertility; d) there was an unmet need for contraception (11.0% for birth spacing and 8.5% for terminal methods) (Table 3.5.4). Other studies have estimated that about one sixth of all pregnant women seek abortion because they do not want continuation of pregnancy. Illegal induced abortion continues to be a major cause of maternal morbidity and mortality (Figure 6).
 3.5.31
During the Ninth Plan period the Family Welfare Programme will be geared
up to meet the unmet demand for contraception with the twin objectives
of reducing maternal morbidity and mortality and achieving rapid decline
in birth rates. Data from the National Family Health Survey indicate
that apart from place of residence education influences IMR, TFR and
CPR (Figure 7).
3.5.31
During the Ninth Plan period the Family Welfare Programme will be geared
up to meet the unmet demand for contraception with the twin objectives
of reducing maternal morbidity and mortality and achieving rapid decline
in birth rates. Data from the National Family Health Survey indicate
that apart from place of residence education influences IMR, TFR and
CPR (Figure 7).
3.5.32 The increased awareness of educated urban population and access to FW services are likely to be the major factors responsible for this.
Inter-State/ intra-State differences in Fertility and Mortality
3.5.33 In spite of the uniform national norms set under the 100% Centrally Funded and Centrally Sponsored Scheme (CSS), there are substantial differences in the performance between States as assessed by IMR and CBR (Table 3.5.1). At one end of the spectrum is Kerala with mortality and fertility rates nearly similar to those in some of the developed countries. At the other end, there are the four large northern States (Uttar Pradesh, Bihar, Madhya Pradesh and Rajasthan) with high Infant Mortality Rate and Fertility Rates. During the Ninth Plan special efforts will be made to achieve rapid reduction in IMR and meet all the felt needs for contraception in these four States.
3.5.34 As the availability and utilisation of family welfare services is the critical determinant of performance in Family Welfare Programme, achievements in terms of reduction in IMR and CBR go hand in hand in most States. However, there are exceptions; both Punjab and Tamil Nadu have good primary health care infrastructure; IMR in both the States are identical and the age at marriage in these States is similar; TFR in Tamil Nadu is 2.1 and in Punjab it is 2.9 (Table 3.5.1). In Bihar, IMR is 72 and TFR is 4.6 but Assam with IMR of 75 has a TFR of 3.8. During the Ninth Plan, efforts will be made to identify the factors responsible for poor achievements in terms of IMR and TFR and area specific remedial measures will be planned and implemented in the States.
3.5.36 District wise data on CBR and IMR computed on the basis of Census 1991 show that there are marked differences in these indices not only between States but also between districts in the same State. Census 1991 has confirmed that even in Kerala there are districts where IMR (Idikki) and CBR (Mallapuram) are higher than national levels. There are districts in UP with IMR (Almora) and CBR (Kanpur -Urban) lower than national levels. The Family Welfare Programme, therefore, has been re-oriented to (a) remove or minimise the inter and intra-state differences, (b) undertake realistic PHC based decentralised area-specific microplanning tailored to meet the local needs and c) involve Panchayati Raj institutions in programme development and monitoring at local level to ensure effective implementation of the programme and effective community participation.
3.5.37 States like Kerala and Tamil Nadu have achieved low CBR and IMR at relatively low cost (Table 3.5.5). On the other hand, States like Haryana and Punjab have not achieved any substantial reduction in CBR in spite of higher expenditure per eligible couple. In States like Bihar and Uttar Pradesh the expenditure is low and performance is poor. In between these extreme categories are States like Orissa and Andhra Pradesh with average or below average expenditure and average or below average performance in MCH or family planning. In some States like Orissa and West Bengal the performance in family planning is better than the performance in MCH or vice versa. During the Ninth Plan, the recommendation of the NDC Committee on Population, that factors responsible for observed differences in utilisation of funds as well as impact of the programme should be studied and existing lacunae rectified not only at the State but also at the the district level will be implemented.
3.5.38 It is noteworthy that States like Kerala and Tamil Nadu (where sterilisation is the most commonly utilised method of contraception) have been able to achieve Total Fertility Rate (TFR) of 2.1 even before CPR of 60 has been achieved and that the cost of family welfare programme per eligible couple in these States is relatively low. Given the fact that most couples in India complete their family by the time they are in their mid-20s and marriage is a socially stable institution, sterilisation is the most logical, safe and cost effective contraception to protect these young couples against unwanted pregnancies.
 3.5.39 Over the last two decades there has been a steep fall in number
of vasectomies (Figure 8). At the moment, over 97% of all sterilisations
are tubectomies. If, over the next decade, attempts are made to repopularise
vasectomy so that this safe, simple procedure forms at least 50% of
all sterilisations there will be a further substantial reduction both
in the morbidity/ mortality and in the cost of permanent methods of
contraceptive care.
3.5.39 Over the last two decades there has been a steep fall in number
of vasectomies (Figure 8). At the moment, over 97% of all sterilisations
are tubectomies. If, over the next decade, attempts are made to repopularise
vasectomy so that this safe, simple procedure forms at least 50% of
all sterilisations there will be a further substantial reduction both
in the morbidity/ mortality and in the cost of permanent methods of
contraceptive care.
3.5.40 In States like Punjab where nearly half of the acceptors of contraception are using temporary methods such as IUD and Condoms (CC) the cost for family welfare programme per eligible couple is high. In addition, in spite of the relatively high couple protection rate (CPR), the birth rate continues to remain relatively high. This is most probably because of the low continuation rate of IUD and low use effectiveness and continuation rates for conventional contraception. In these States emphasis during the Ninth Plan will be on providing adequate counseling, offering appropriate contraceptive choices through balanced presentation of advantages and disadvantages of various contraceptive methods so that the couple can make a choice of contraceptives; these initiatives will improve continued use of contraceptives and reduction in unwanted births. Adequate follow up care and counselling will also be provided.
3.5.41 Kerala, the first State to achieve TFR of 2.1 did so in spite of relatively low per capita income, whereas in spite of having substantially higher per capita income Punjab and Haryana are yet to achieve TFR of 2.1. Obviously, in Indian context, economic development and increase in per capita income are not essential prerequisites for achieving reduction in fertility. Tamil Nadu was the next State to achieve TFR of 2.1. It did so in spite of higher IMR and lower female literacy rate than Kerala; Maharashtra, which has similar IMR, is yet to reach a substantial decline in TFR. This shows that in some States the decline in IMR is not also a critical determinant of decline in fertility. Andhra Pradesh is likely to achieve TFR of 2.1 by the end of the Ninth Plan. The State has shown a steep decline in fertility in spite of relatively lower age at marriage, low literacy and poorer outreach of primary health care infrastructure. Haryana and Punjab, which have comparatively higher age at marriage, higher literacy rate and better outreach of primary health care infrastructure, have not succeeded in achieving a similar decline in fertility rates.
3.5.42 Both Kerala (in 1989) and Tamil Nadu (in 1993) achieved TFR of 2.1 long before the CPR of 60 was reached. In both these States sterilisation was the major mode of contraception, suggesting that under conditions prevailing in these States the low utilization of spacing methods was not a hindrance for the achievement of replacement level fertility. Andhra Pradesh is on the thereshold of achieving replacement level of fertility. UT of Goa and Pondicherry have been having less than replacement level fertility for over a decade.
3.5.43 Kerala’s achievement TFR 2.1 inspite of low per capita income, disproves the theory that economic development is an essential prerequisite for reduction in fertility. High status of women, female literacy, age at marriage and low infant mortality were thought to be the factors behind the rapid fall in fertility in Kerala. Tamil Nadu, the next state to achieve TFR of 2.1 did so inspite of relatively high IMR, low literacy and low per capita income. Andhra Pradesh is experiencing a rapid decline in fertility inspite of low literacy, low age at marriage, high IMR and low per capita income. Studies to find out the basis of this rapid demographic transition are underway.
3.5.44 The experience of these three States have clearly shown that in the Indian context it is possible to achieve replacement level of fertility inspite of adverse socio-economic and demographic indices. It is noteworthy that analysis of districtwise data clearly shows that in every State there are districts with excellent performance in MCH and FP. It is in this context that the Ninth Plan document visualises district based de-centralised planning wherein each State can replicate in all other districts the success that some districts had achieved. The NFHS has unequivocally shown that there is substantial unmet need for contraception in all States; the focus will therefore be on ensuring that these needs are fully met through mechanisms that are appropriate in the local context.
3.5.45 Health professionals believe that availability and access to family welfare services is one of the critical determinant of decline in fertility. In the North-eastern States of Tripura, Manipur, Mizoram there is substantial difficulty in accessing primary health care facilities, but these States have achieved not only low fertility rates but low infant mortality, suggesting thereby that a literate population with awareness can successfully overcome the deficiency in access to and availability of primary health care infrastructure. In spite of constraints of infrastructure, manpower and financial resources, high illiteracy and marked diversity between States, the Family Welfare Programme has, during the last five decades succeeded in achieving substantial reduction in infant mortality and fertility rates within the framework of the democratic set-up. In this process the Family Welfare Programme has shown that factors such as economic status, educational status, access to health services which were thought to be essential prerequisites for achieving sustained decline in birth rates are not necessarily so for reduction in birth rate in the Indian context. The experience of different States, while implementing family welfare programme clearly shows that the programmes can succeed despite limitations in several States. The need for identifying the local problems and also methods by which these could be overcome from within the resources available is, therefore, of paramount importance in rapidly bringing down infant mortality and high fertility. The Ninth Plan's emphasis on area-specific assessment of the need and micro-planning is expected to provide the policy direction for achieving this goal.
|
Eighth Plan Targets and Achievements Indicator Targets Achievements CBR 26 27.4 (SRS 1996) IMR 70 72 (SRS 1996) CPR 56% 45.4% (March 1997) |
Performance during the Eighth Plan
3.5.46 During the Eighth Plan the Crude Birth Rate (CBR) and Infant Mortality Rate (IMR) declined to 27.4 and 72 against the targets of 26 and 70 respectively. The Couple Protection Rate (CPR) increased to 45.4% against the target of 56% during this period. The target for IMR is achievable; target for CBR may be difficult to achieve; the target for CPR has not been achieved.
3.5.47 The performance of the Family Welfare Programme in terms of achievements of targets in contraception, immunisation, anaemia and Vit.A prophylaxis programmes during the Eighth Plan, is given in Table 3.5.6. Between 1992 and 1996 the number of sterilisation has remained unaltered. There has been an increase in IUD and OC use till 1995-96 and CC use till 1994-95. Whenever such a massive shift is attempted, the system requires a major preparatory effort, including sensitisation of health care providers through intensive training and even then it may take some time to adapt to the change. Comparison of the performance between 1995-96 and 1996-97, (after the abolition of method-specific targets) indicate that at the national level there has been a reduction in the acceptance of different methods of contraception. The fall in condom use during 1995-96 and 1996- 97 might, at least in part, be attributable to reduction in wastage. Comparison of the performance between 1995-96 and 1996-97 shows that there are substantial differences in performance between States. Tamil Nadu, Karnataka, Rajasthan have shown an improvement in acceptance of sterilisation as well as IUD. It is a matter of concern that poorly performing States like Bihar and UP have shown a further decline upto 50% in performance. Efforts to gear up the system and minimise the time lag in adopting to the decentralised planning and implementation are under way.
3.5.48 The coverage under the anaemia and Vit A prophylaxis programme has shown substantial improvement but is still way below the target of 100 per cent. Adequate supply of these drugs and continued intake at appropriate time will be attempted during the Ninth Plan.
3.5.49 During the Eighth Plan, the coverage under the immunisation programme was maintained. However the target of 100% coverage by 1997 is unlikely to be achieved for all the six Vaccine Preventable Diseases (VPD). There has been a substantial improvement in the quality of the programme but even now there are slippages in the programme resulting in occasional morbidity and rare mortality. These will be eliminated during the Ninth Plan period. The Pulse Polio initiative to eradicate polio by 2000 AD and special school health check up programme were taken up during the Eighth Plan period. Pulse Polio programme will be continued until the elimination of Polio is achieved. During the Eighth Plan there has been a progressive fall in the reported cases of diphtheria, measles, polio, tetanus and pertussis. However, under-reporting and under/ over-diagnosis continue to occur. VPD surveillance, especially for poliomyelitis, will be strengthened throughout the country during the Ninth Plan.
3.5.50 Even though the targets set for IMR and CDR are likely to be achieved, it is noteworthy that maternal, perinatal, neonatal (Figures 6 and 9) mortality rates continue to remain high. This is because the components of antenatal, intrapartum and neonatal care programmes are not aimed at universal screening of risk factors for identification and appropriate referral of the `at risk' individuals. Improvement in the contents and quality of antenatal and paediatric care at primary health care level will receive focussed attention during the Ninth Plan.
3.5.51 To sum up the basic premises of the Family Welfare Programme from inception has been that:
Basic
premises of the Family Welfare Programme are:
|
-
the programme will provide integrated Maternal and Child health (MCH) services and contraceptive care;
-
acceptance of family welfare is voluntary,
-
the Government’s role is to create a favourable environment for the people to adopt small family norm, by improving awareness through information and education and ensuring easy and convenient access to family welfare services free of cost.
|
Lessons learnt during implementation of FW programme:
|
Next >>